Ventral Slot Surgery Recovery
- Ventral Slot Surgery Recovery Kit
- Ventral Slot Surgery Recovery
- Ventral Slot Surgery Recovery Centers
- Ventral Slot Surgery Recovery Disk
- Ventral slots alter the vertebral range of motion at the surgical site which can lead to instability and subluxation. Postoperative care of the ventral slot patient involves cage rest for most of the day with monitored leash walks using a body harness.
- Dog presented for neck pain. A massive C3-4 disc was discovered. A C3-4 ventral slot is being live streamed at 4:00 pm.
(n = 31), caudal (n = 125) or both (n = 5) types of myelography at the same time, and surgery - ventral slot decompression (SLOT) (n = 18) or hemilaminectomy (n = 143). During the post-surgical period we observed seizures, GIT complications, cystitis, and surgical wound healing problems or even death of the patients. After surgery, your pet should lay low for six to eight weeks. The spinal cord recovers slowly and extra care must be taken not to allow running, jumping, stairs, playing with other dogs, or hopping on or off furniture. Physical therapy can be started right after surgery to help regain strength. Can dogs re-injure themselves after surgery?
A triple ventral slot decompression surgery was performed. The dog regained ambulation after surgery with only mild deficits remaining. © 2017, Israel Veterinary Medical Association.
MENU
Abstract – Treatment and Prognosis
Treatment
Surgical Treatment
Direct Access Decompression
Indirect Decompression
Domino Lesion or Adjacent Segment Disease
Direct Decompression with Distraction and Dynamic Stabilization
Advantages of Cervical Disc Arthroplasty versus Standard Surgical Techniques
Conclusion
Bibliography
Abstract – Treatment and Prognosis
Bone associated wobbler syndrome (BAWS) and disc associated wobbler syndrome (DAWS) in dogs can be treated either medically or surgically. However, both conditions are considered surgical diseases and medical conservative treatment is associated with a guarded prognosis. While for BAWS direct spinal cord decompression through a dorsal laminectomy or hemilaminectomy seems to be the best way to treat this disease process, the ideal surgical procedure for DAWS still does not exist. Preliminary clinical studies are showing that cervical disc prosthesis may be a valuable method to treat DAWS in dog.
Treatment
Medical treatment
Medical treatment for dogs affected by DAWS and BAWS is similar. Activity restriction and corticosteroids may be indicated in a normal dog with a first episode of neurologic deficits following minor trauma; otherwise, surgery is the treatment of choice. Conservatively treated dogs should have activity restriction for at least two months – they can be walked on leash (preferably attached to a chest harness rather than a collar), but free unsupervised activity should be avoided. This is to minimize high impact activities that could exacerbate the dynamic component of spinal cord compression. Corticosteroids at an anti-inflammatory dose (prednisone 0.5 mg/kg every 12 hours) tapered over 2 to 3 weeks has been recommended.1 Alternately, dexamethasone (0.2 to 0.25 mg/kg every 24 hours [not to exceed 8 mg/dog] initially for 1 to 3 days depending on the severity of the clinical signs, and then continue with 0.1 mg/kg every 24) has also been recommended.1 A gastrointestinal protector such as famotidine (0.5 mg/kg every 12-24 hours) or omeprazole (0.7 mg/kg every 24 hours) may be used in conjunction with corticosteroids. However, due to the many side effects of corticosteroid, their prolonged use is not recommended. Nonsteroidal anti-inflammatory drugs (NSAIDs) may be used when corticosteroids are contraindicated or when clinical signs are limited to cervical pain. The use of corticosteroids is more indicated in patients with more severe neurologic signs (ataxia, paraparesis or tetraparesis), and their ability to reduce interstitial spinal cord edema may have some prognostic value in establishing the reversibility of the spinal cord lesion. Physical therapy and electroacuncture have also been reported. 2,3 Recent studies that evaluated non-surgical or surgical treatments reported that 81% of the dogs treated surgically (via ventral slot, dorsal laminectomy, or distraction and fusion) improved, while 54% and 45% of dogs, respectively, improved with medical treatment.4-6 In a more recent study, conservative medical treatment provided long-term improvement for only 38% of dogs.7 These studies concluded that conservative treatment for DAWS is associated with a guarded prognosis.4-6 Importantly, the neurologic status of dogs at 1 month after diagnosis of DAWS seems to be critical for determining the outcome of conservative medical treatment. In all dogs in which conservative medical treatment was unsuccessful, the neurologic condition had deteriorated at 1 month after diagnosis of DAWS. In these dogs, deterioration of clinical status was generally rapid and progressed to tetraplegia within 6 months after diagnosis.7 Therefore, evaluation of neurologic condition at 1 month after diagnosis of DAWS is essential to identify the patients in which the clinical condition is likely to deteriorate to a non-ambulatory status without surgical intervention. This may be used as a prognostic indicator and for earlier identification of surgical candidates, before the spinal cord damage becomes irreversible.7
Surgical Treatment
Many surgical techniques have been described to treat DAWS, while the surgical options for BAWS are still limited. The surgical techniques can be broadly divided into three categories:
a) direct access decompression,
b) indirect decompression by ventral distraction-stabilization-fusion
c) direct decompression with distraction and dynamic stabilization.
Reported results for surgical treatment of DAWS are summarized in table 1.
Ventral Slot Surgery Recovery Kit
Direct Access Decompression
a) Dorsal laminectomy
This technique is primarily indicated for dogs with BAWS with dorsal or dorsolateral spinal cord compression.8 Dorsal laminectomy is the least commonly used surgical technique for dogs with DAWS, but it may be indicated for dogs with DAWS with compression in multiple spaces. It can be performed by a continuous dorsal laminectomy (usually from C4 to C7) or by single dorsal laminectomy at the affected site.8-10 The major disadvantages of this technique are (a) that the ventrally located disc material cannot be removed, and (b) there may be significant, short-term morbidity with deterioration of neurologic status leading to considerable nursing problems (Fig. 1).
This technique requires an extensive soft-tissue approach, and ventrally located disc cannot be removed. The decompressed spinal cord (multiple arrows) is visible after the removal of the dorsal lamina and the interarcuate ligaments of the affected vertebrae. The degenerated articular facets (asterisks) are also visible.(A) Same dog of Fig. A requiring intense post-operative nursing care.(B)
In one study, which included dogs affected by BAWS and DAWS, post-operative morbidity was high and 70% of dogs had worsened neurologic status 2 days after surgery. This immediate post-operative decline was attributed to transient instability. This may be a negative factor, particularly in dogs with DAWS, which already have a degree of instability at the affected intervertebral space(s) as part of the disease pathogenesis. Surgical removal of the dorsal portion of the vertebrae and ligamentous tissue may result in further instability that would likely manifest as clinical worsening. However, clinical improvement is expected to follow the initial deterioration as the area re-stabilizes over time. Furthermore, the dorsal approach requires extensive soft tissue dissection, which produces significant tissue trauma and post-operative edema, a contributing factor to the high morbidity.8 Post-operative complications, including decubital ulcers, seroma formation and recurrence of clinical signs have been reported in 30% of dogs with a mean length of hospitalization of 8.3 days.8 Formation of a laminectomy membrane at the surgical site may cause restrictive fibrosis during healing, which is mostly responsible for delayed recurrence of neurologic signs.8 However, in two separate studies, dorsal laminectomy was reported to be successful in providing long-term improvement in the post-operative neurologic status in 19 of 20 dogs and in 11 of 14 dogs, respectively.8,11 For dogs that become or remain non-ambulatory after surgery, it has been reported to take an average of 2.5 months to regain ambulatory status without assistance. The mortality rate related to euthanasia performed secondary to recurrence of clinical signs is 15%.8 In the author’s experience, dogs with BAWS treated with dorsal laminectomy tend to have a shorter post-operative recover time and a better outcome than dogs affected by DAWS treated with this technique.
b) Hemilaminectomy
Cervical hemilaminectomy in dogs through a modified lateral approach has been reported to facilitate treatment of lateralized and foraminal cervical spinal lesion associate with BAWS, DAWS, as well other cervical spinal diseases.12 None of the 16 dogs in this study had post-operative deterioration in neurologic status. Outcomes were good to excellent in 2 dogs with BAWS and 1 of the 2 dogs with DAWS. Hospitalization, time to optimal recovery, and overall outcome were not different from previously reported results using other surgical approaches to treat analogous neurologic conditions. Although the long-term follow up was not available for all patients in this study, outcomes were generally favorable.
c) Ventral slot
Ventral slot is the surgical technique primarily indicated for single ventral static compressions, and there is extensive experience with its use.1,13 In the standard ventral slot technique, the slot should not exceed one-third of the length and width of the vertebral body (Fig. 2).
A slot is performed between the two vertebrae until the protruded disc with the associated thickened ligaments are reached and removed. The slot should not exceed one third of the length and width of the vertebral bodies. After decompression, nothing usually is placed to fill the slot and fusion may occur in 6-8 weeks. Alternatively, to promote fusion, a cancellous bone graft harvest from the head of humerus may be packed in the slot.
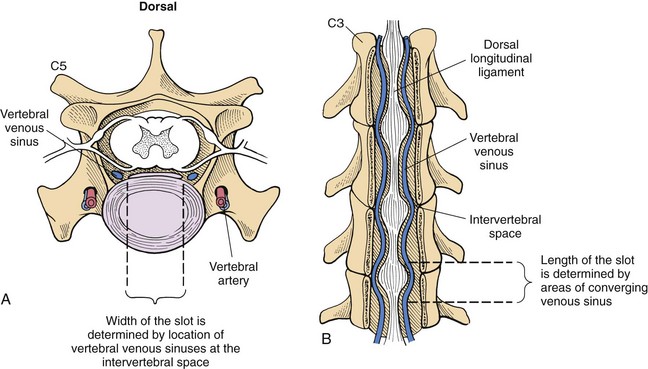
All disc protrusion and hypertrophic ligament should be removed to effectively decompress the spinal cord. The ventral slot technique when properly performed offers adequate spinal decompression, and fusion is expected to occur between 8 and 12 weeks after surgery.1 However, ventral decompression can be technically challenging and can exacerbate vertebral instability. Bleeding from the internal vertebral venous plexus is a major complication of ventral slot decompression and care should be exercised to avoid injuring this structure. If bleeding occurs, it can prolong surgery considerably, can lead to incomplete spinal cord decompression, and if profound may require cessation of the surgery and blood transfusion.14 Ventral slot decompression may also result in further collapse of the disc space and worsening of the spinal cord compression because of additional in-folding of the ligamentous structures and joint capsules. Post-operative complications occurred in over 20% of DAWS patients treated with a ventral slot.15,16 Collapse of the intervertebral space can also compress the nerve roots and radicular arteries in the intervertebral foramen, which can cause cervical pain and focal spinal cord ischemia. Vertebral subluxation and death shortly after surgery have been also reported.16,17 The recovery rate after standard ventral slot decompression has been reported to be 4 to 6.5 weeks.14,16 Duration of hospitalization stay and the mean time necessary to reach optimal neurologic status is similar to the dorsal decompression technique.16 This technique has been reported to be clinically effective, with an average long-term success rate of 72%.15,16,18 This is most likely attributable to fusion occurring at the treated space post-operatively.15,19 It is likely that fusion resolves the vertebral instability and promotes the reduction of the remaining thickened ligamentous structures.
A modification of the traditional ventral slot is the inverted cone slot which maximizes spinal canal exposure with the aims of minimizing the risks of hemorrhage and subluxation. The slot resembles an inverted cone in which the base of the cone lies adjacent to the ventral vertebral canal.1 Two or more slots for the treatment of multiple ventral compressions can be performed, but the risks of complication are higher.1
Indirect Decompression
Distraction-stabilization techniques
Several techniques have been described to provide distraction and stabilization for treatment of DAWS. Distraction-stabilization techniques distract the vertebrae to stretch the thickened ligamentous structures and relieve spinal cord compression. The vertebrae are then stabilized with appropriate implants and fusion is promoted with bone autograft (cancellous, cortical or corticocancellous)4 or allograft.19 Various techniques have been used to maintain distraction and/or graft retention to allow for bony fusion of the affected interspace.4,20-28 The principle advantage of these techniques is the immediate relief of spinal cord and nerve root compression achieved by the distraction. Early implant failure with loss of distraction before bony fusion occurs has been the most common cause of failure in distraction-stabilization techniques. The short-term complication rate for the various distraction-fusion techniques has been reported to range from 10% to 21% and it is frequently associated with implant failure.
a) Distraction stabilization using pins or screws and PMMA
This technique is recommended for single ventral dynamic compressive lesions. A partial or standard ventral slot is performed to alleviate the spinal cord compression, prior to the application of 4 smooth or (preferably) positive profile Steinmann threaded pins or fully threaded screws29 (Fig 3).
After a standard ventral slot and spinal cord decompression, four pins (positive profile Steinmann threaded pins or fully threaded screws preferred) are placed at an angle, two in each vertebral body (A); linear traction is then applied to the intervertebral space, which is then maintained by a bone cement bridge as shown in this immediate post-operative radiographs (B).
The recommended angle of pin or screw insertion is 30 to 35 for the C5 and C6 vertebrae and 45 for the C7 vertebra.22, 30 Vertebral stability is then maintained by application of a polymethylmethacrylate (PMMA) bridge that incorporates the pins or screws. The long term success of this technique is reported to be 73%.22 Bicortical penetration of pins or screws into the vertebral canal with spinal cord damage or vertebral artery or nerve root compromise has been reported to occur in 25% to 57% in experimental studies.29, 30 Other complications include failure of the bone cement bridges, pins, screws or plates, as well as various soft tissue complications, such as esophageal erosion because of ventral hardware or PMMA prominence.4
A novel screw-bar-PMMA fixation implant, consisting of screws inserted into the transverse processes and a U-shaped Steinman pin wired to the screw and covered by PMMA has been described in an experimental study.31 In this study, this technique reduced the incidence of penetration of the transverse foramen or vertebral canal compared with the traditional pin-PMMA implant.
b) Distraction using a PMMA plug.
This technique can be applied for either single or multiple ventral compressions.4,21 After performing a discectomy, distraction is applied (usually by using a modified Gelpi retractor applied in two pre-drilled holes in the ventral cortex of the affected vertebrae), an anchor hole is drilled into the cranial and caudal endplates, and PMMA in the semifluid state (before polymerization) is poured in the slot and in the anchor holes.20 (Fig. 4)
Two holes are created in the cranial and caudal endplates to anchor the PMMA plug (a). Immediate post-surgical radiography showing that the PMMA plug is providing adequate distraction at the treated disc space. The still visible myelogram is showing that the spinal cord is free of compression (b). To promote fusion, a cancellous bone marrow allograft (arrows) collected from both humeral heads is placed along the ventral aspect of the two involved vertebrae covering the PMMA plug (c).
Modification of this technique includes placement of a retention screw or pin ventral to the plug.4 The long-term success rate with this technique is reported to be 82%.21 Complications may include ventral implant migration and consequently distraction failure. The heat generated during polymerization of the PPMA may cause end plate necrosis, with intrusion of the PMMA plug into the vertebra and consequently distraction failure. Another disadvantage of this technique is the required application of a well-padded cervical brace for 8 weeks, which has to be replaced every 2 weeks (or sooner if problems arise). This is not well tolerated by some patients.
c) Distraction-stabilization fusion with locking plates and screws.
This technique is indicated for a single-level traction-responsive DAWS lesion. A few approaches to this distraction-stabilization technique have been described.20,28,32 These include discectomy, distraction of the affected space with a Caspar cervical distractor, inserting in the distracted space either a cancellous bone allograft20 or a cortical ring allograft to promote fusion28, and fixing the vertebrae of the affected site in distraction with the Synthes Cervical Spine Locking Plate (CSLP) (Fig 5).
Titanium single-level small stature cervical spine locking plate and unicortical locking screws (Synthes spine) (A), together with freshly thawed distal femoral cancellous block allograft (Veterinary Transplant Service Inc.) (B), are used to maintain the affected disc space distracted, as shown in the immediate post-operative radiographs (C and D). The block graft is carefully sculpted by mean of high speed air drill to the exact shape and dimensions of the distracted disc space to maintain distraction and to maximize surface area of contact between graft and end plate. Coutesy of Dr. E.G. Trotter; reprinted with permission.20
The disadvantages of these techniques are the high technical abilities necessary, and the cost associated with the plate, the screws and the allograft. This type of plating system is designed for use on the human cervical vertebral column (explaining the high cost), and because the ventral aspect of the canine cervical spine tends to have more variation in shape, additional time and technical ability is needed to contour the ventral surface of the vertebral column, through drilling of the bone, in combination with bending of the spinal plate to fit. The success rate using this technique has ranged from 80% to 83%.20,28 The overall success rate using direct access or indirect decompression is approximately 80% (70% – 90%).1
Domino Lesion or Adjacent Segment Disease
Clinical relapse after initial recovery is a common complication after surgical intervention for DAWS.4,6,33 These episodes are generally caused by the development of a new compressive lesion on the spinal cord at a disc space adjacent to the surgically treated site.34 This is commonly known as a domino lesion or adjacent segment disease. The exact etiopathogenesis of this complication is controversial.35 It is likely that fusion or distraction may increase the risk of a domino lesion. Domino lesions are believed to be the result, at least in part, of abnormal stresses imposed on one intervertebral space by fixation of an interspace adjacent to it. These stresses can exacerbate any pre-existing subclinical instability, and reproduce the same problem at an adjacent disc space4,36 (Fig. 6).
MRI (T2-weighted sagittal) one year post-surgery, in a 7 year-old Doberman surgically treated for DAWS at C6-C7. The dog was treated with distraction fusion using a cortical bone graft and stabilized with titanium screws. The dog presented one year later with chronic progressive tetrapatesis. New compressive “domino” lesions, likely as consequence of the fusion at the treated site, are evident at C5-C6 ventrally, and at C4-C5 and C3-4 dorsally (arrows). Courtesy of Dr. G. Destrero
Some others believe that the development of the adjacent segment disease is part of the natural progression of the disease, and if this is true DAWS should be considered a multifocal disease.35 Recurrence of clinical signs secondary to a domino lesion may occur as a late post-operative complication with any of the above described techniques. Recurrence of paraparesis or tetraparesis occurs in up to one-third of dogs after either ventral slot or metal implant and bone cement fixation, mainly with distraction-stabilization techniques.1 It usually occurs between six months and four years after the original surgery, with a mean recurrence of around two years.16,37 A meta-analyis of dogs treated surgically for DAWS revealed an 80% short-term success rate with about 20% of successful surgeries having significant recurrence after long-term follow-up.35 The type of surgery performed (decompression versus distraction-fusion) did not influence the outcome. Because MRI may allow early identification of the adjacent intervertebral space at risk of developing a domino lesion, treatment of the affected and/or suspected adjacent intervertebral disc space may be recommended to reduce the incidence of domino lesions.4,21,26 Given the high rate of surgical failure and long term recurrence, new methods are continually investigated for the treatment of DAWS in dogs.
Direct Decompression with Distraction and Dynamic Stabilization
Cervical Disc Arthroplasty
Cervical disc arthroplasty is a novel technique and it is mainly indicated for dogs with DAWS with single or multi-level traction-responsive spinal cord compression. 37,38 The goals of this technique are to provide distraction and greater stability, while preserving motion after neural decompression. This technique includes ventral spinal cord decompression via a discectomy, minor burring of the vertebral end-plates (more of the caudal end-plate) to accommodate the implant, and placement of an artificial disc, which is specifically designed and manufactured for the dog’s cervical spine. 37-39 (Figs. 7-11).
The prosthesis is made of a titanium alloy, and consists of two end-plates, with a range of movement of 30o between the plates. This prosthesis is rotationally unconstrained, following the ball-end-socket principle, and independent of supplemental fixation. The concavity and convexity of the central aspects of the end plate surfaces result in a ball-and-socket type of connection between the end plates. The articulated ball is made of PolyEtherEther-Ketone (PEEK) to avoid metal-to-metal friction. The external surface of each-endplate is convex resembling the concavity of the caudal end plate of the most caudal cervical vertebrae. The outer surface of each end plate has concentric grooves and is pre-treated with a dual acid etch bath to promote bone ingrowth into the prosthesis. Six standard sizes of prosthesis are available, labeled S1, S2, S3, and M1, M2, and M3. Two end-threaded stainless pins and a barrel holder are used to hold together the two pieces of the implant during placement within the disc space. The threaded end of the pin is screwed into each piece of the implant (A). After the two pieces of the implant are assembled, the two pins are inserted into the barrel holder (B). A burr resembling the external convexity of the prosthesis is custom made for milling the slot to precisely accommodate the external convexity of the implant within the slot (C). A twenty-degree angle attachment for the high-speed air drill is used to facilitate burring at an angle parallel to the disc space (D). The barrel holder has the double function of holding the prosthesis assembled with one extremity (E) and to unscrew the end-threaded pins after the prosthesis is placed in the slot with the other extremity.
After routine surgical preparation, the ventral aspect of the affected vertebral bodies is accessed via a standard approach as for a ventral slot procedure. A discectomy is performed across the intervertebral space. A self-retaining Caspar distractor is placed and maintained distracted to allow the final cleaning of the disc space and the subsequent burring with the dedicated burr (A). The prosthesis is inserted while maintaining the Caspar distractor in maximal distraction. Gentle pressure is applied to force the implant into the slot, and an audible click is usually heard when the convex area of the implant slips past the edge of the slot (B). To ensure that the implant is seated (as much as possible) on the midline, the barrel holder is rotated until the fissure of its proximal end is aligned with the long axis of the vertebrae (C). After implantation, the distraction is released, allowing the two vertebral end-plates to collapse on the prosthesis. After assessing that the prosthesis is correctly seated in position, in order to ensured that the implant is firmly in position, the two pins still screwed in the prosthesis are grasped with a needle holder and upward traction is applied in an attempt to dislocate the prosthesis from the slot. Once the surgeon is satisfied that the prosthesis is held snuggly between the vertebrae, the two pins are unscrewed from the two prosthetic end-plates, and the two Caspar distractor pins are removed from the vertebral bodies. Bone wax or gel foam is placed to stop the bleeding that might occur at the holes created by the two Caspar distractor pins. The longus colli, sternohyoideus, and sternocephalicus muscles and subcutaneous and subcuticular tissues are then closed in a routine manner. Courtesy of Wiley-Blackwell; with permission.
Intraoperative photo (A), and immediate post-operative radiographs (B and C), of the same dog in Fig 1 affected by disc associated wobbler syndrome at C3-C4 and C5-C6, and with a suspected congenital vertebral fusion at C4-C5. Multiple cervical disc arthroplasty was recommended to avoid additional fusion at the affected spaces, which, in addition to the pre-existing one, could have had predispose the patient to a domino lesion at C6-C7. Nine months post-operative radiographs in lateral (D) dorsiflexion (E) ventroflexion (F) and ventro-lateral (G) showed mild decrease of the original vertebral distraction, no heterotopic ossifications and retaining of mobility at both treated spaces. This dog presented with a four months history of progressive ataxia/tetraparesis and regained a full neurological function.
MRI T2 weighted of 6 year-old Doberman with a two-year history of ataxia/tetraparesis treated with NSAID who presented with acute tetraplegia; the MRI showed multi-level DAWS lesion at C5-C6 and C6-C7 (A). The dog was treated with double cervical disc replacement and the immediate post-operative radiograph showed adequate disc placement at both treated sites (B). The dog became ambulatory two weeks post-surgery and neurologically normal four months later. (C). At seven months follow up post-operative radiographs showed decreased of the immediate post-surgery vertebral distraction and heterotopic ossification at both treated spaces Mobility was not detectable at C6-C7 and significantly decreased at C5-C6. (D). However, this didn’t affect the clinical out-come. The dog continued to maintain his normal neurological status without any adjuvant anti-inflammatory or anti-pain medication.
MRI T2 weighed of a 12 year-old Dalmation with a six-month history of ataxia/tetraparesis unresponsive to corticosteroids; the MRI showed multi-level DAWS lesion at C3-C4, C4-C5 and C5-C6. The dog was treated with triple cervical disc replacement and the immediate post-operative radiograph showed adequate disc placement at both treated sites. One day post-op, he dog’s neurological status was not worse than the pre-operative status. The dog was still ambulatory, appeared comfortable and was sent home one day post-surgery.
Cervical disc arthroplasty has the potential to achieve the optimal goals of spinal cord and nerve root decompression, restoration of the biomechanics at the surgically treated sites, sparing the adjacent disc spaces from the alterations in loading associated with the standard ventral slot and distraction-fusion surgical techniques, and potentially preventing the occurrence of a domino lesion. Experimentally, pre-clinical studies of this technique showed that canine cervical spines with this implanted prosthesis had biomechanical behaviors (i.e. flexion, extension, lateral bending, and torsion) similar to an intact spine when compared to cervical spines treated with ventral slot or PMMA distraction-fusion techniques.39 In two separate clinical studies, cervical disc arthroplasty was well-tolerated and all dogs had immediate post-operative recovery with adequate degree of distraction in the immediate post-operative radiographs.37,38 In the majority of dogs, the distraction was moderately lost over time; though at a median follow-up of 15 months this was not clinically significant.38 Cervical disc arthroplasty, similar to ventral slot, allows direct spinal cord decompression at the affected site(s).37,38 Similar to distraction-fusion techniques, cervical disc arthroplasty provides immediate distraction at the treated site(s), which further decreases any residual compression from the redundant ligamentous structures, and relieves spinal cord ischemia caused by compression of the vertebral spinal artery. The reopening of the narrowed intervertebral foramina further decompresses the nerve roots, eliminating recurrent cervical pain.
Advantages of Cervical Disc Arthroplasty versus Standard Surgical Techniques
The advantage over the standard ventral slot is that the artificial disc acts as an internal spacer, preventing the early collapse of the intervertebral disc space that is usually associated with ventral slot. The advantage over pins or screws and PMMA distraction-fixation techniques is the elimination of the potential complications associated with pin impingement on neurovascular structures.37 The advantages over the distraction and fusion with plate and screws are that the artificial disc is a self-anchoring device that doesn’t require the expensive surgical equipment and cost associated with plating two vertebrae, and the elimination of the potential complications associated with failure of these implants.37 Additional advantages of arthroplasty over these technique are that the prosthesis is relatively easy to implant, is cost-effective (its cost may be equivalent to the cost of the pins and PMMA, and significantly less compared to the locking plate-fusion techniques), doesn’t require special instrumentation used for plating, and can be applied to multiple sites if needed. This is particularly important in the event of multiple lesions or when signs of mild spinal cord impingement are evident at adjacent intervertebral disc spaces during MRI.37 Cervical disc replacement is less invasive than traditional surgeries, reduces the risks and failures of more common surgical techniques, and it is associated with a faster post-operative recovery. Dogs that are ambulatory prior to surgery are expected to be ambulatory after surgery, and thereby this technique can even be performed on an outpatient basis. Lastly, the possibility of performing MRI studies after implantation of this titanium prosthesis, without interfering with spinal cord visibility, is a distinct advantage over many other distraction stabilization techniques.37 In the event of recurrent clinical signs, this allows accurate re-evaluation of the spinal cord at the treated site as well as adjacent locations.37
Possible complications associated with this type of cervical arthroplasty, similar to those reported in humans, include subsidence (sinking of the implant into the softer cancellous bone of the vertebral body), heterotopic ossification and ankylosis at the treated sites, and prosthesis migration.37,38
Ventral Slot Surgery Recovery
Conclusions
Disc associated Wobbler syndrome and bone associated Wobbler syndrome are relatively common causes of chronic spinal cord compression in adult large breed dogs. DAWS and BAWS are considered surgical diseases. While for BAWS direct spinal cord decompression through a dorsal laminectomy or hemilaminectomy seems to be the best way to treat this disease process, the ideal surgical procedure for DAWS still does not exist. Preliminary clinical studies are showing that cervical disc prosthesis is a valuable method to treat single and multilevel DAWS lesions in dogs. By preserving the motion segment, arthroplasty represents an attempt to prevent adjacent segment degeneration while treating the underlying disease. Because of the minimal morbidity and many other advantages of this technique, use of cervical arthroplasty may increase owners’ willingness to pursue the surgical treatment of their pets.
Bibliography
1. da Costa RC. Cervical Spondylomyelopathy (Wobbler syndrome). In R. da Costa, eds.Veterinary Clinics of North America, Small Animal Practice, Spinal Diseases. Philadelphia, PA: Elsevier. 2010; Vol. 40, pp. 881-913.
2. Speciale J, Fingeroth JM. Use of physiatry as the sole treatment for three paretic or paralyzed dogs with chronic compressive conditions of the caudal portion of the cervical spinal cord. J Am Vet Med Assoc 2000; 217(1): 43-49 29.
3. Sumano H, Bermudez E, Obregon K. Treatment of wobbler syndrome in dogs with electroacupuncture. Dtsch Tierarztl Wochenschr 2000;107(6): 231-235
4. Sharp N, Wheeler S. Cervical spondylomyelopathy. In W. S. Sharps N, Small animal spinal disorders, diagnosis and surgery Edinburg 2nd ed: Elsevier Mosby. 2005; 211-246.
5. da Costa RC, Parent JM. Outcome of medical and surgical treatment in dogs with cervical spondylomyelopathy: 104 cases (1988-2004). J Am Vet Med Assoc 2008; 233: 1284-1290.
6. De Decker S, Bhatti S, Dechateau L, et al. Clinical evaluation of 51 dogs treated conservatively for disc associated wobbler syndrome. J Small Anim Pract 2009; 50: 136-142.
7. De Decker S, Gielen IMVL, Duchateau L et al. Evolution of clinical signs and predictors of outcome after conservative medical treatment for disc-associated cervical spodylomyelopathy in dogs. JAVMA 2012; 240:7; 848-857.
8. De Risio L, Munana K, Murray M, et al. Dorsal laminectomy for caudal cervical stenotic myelopathy: post-operative recovery and long term follow-up in 20 dogs. Vet Surg 2002; 31: 418-427.
9. Lyman R. Continuous dorsal laminectomy for the treatment of caudal cervical instability and malformation. ACVIM Forum Proceeding. Lakewood (CO): American College of Veterinary Internal Medicine; 1989. P 13016
10. Nanai B, Lyman R, Bichsel P, et al. Intraoperative use of ultrasonography during continuous dorsal laminectomy in two dogs with caudal cervical vertebral instability and malformation (‘wobbler syndrome”). Vet Surg 2006; 35, 465-469.
11. Lipsitz D, Levitski RE, Chauvet AE, et al: Mahnetic resonance imaging features of cervical stenotic myelopathy in 21 dogs. Vet Radiol Ultrasound 2001; 42: 20-27.
12. Rossmeils JH Jr, Lanz OI, Inzana KD, et al. A modified lateral approach to the canine cervical spine: procedural description and clinical application in 16 dogs with lateralized compressive myelopathy or radiculopathy. Vet Surg 2005; 34(5) 436-444.
13. Chambers JN, Oliver Jr JE, Kornegay JN, et al. Ventral decompression for caudal cervical disc herniation in large- and giant breed dogs. J Am Vet Med Assoc 1982; 180: 410-414.
14. McCartney. Comparison of recovery times and complication rate between a modified slanted slot and the standard ventral slot for the treatment of cervical disc disease in 20 dogs. Journal of Sm Anim Pract 2007; 48,498-5001
15. Chambers JN, Oliver J, Bjorling D. Update on ventral decompression for caudal cervical disc herniation in Doberman Pinschers. J Am Anim Hosp Assoc 1986; 22:775-778.
16. Rusbridge C, Wheeler S, Torrington AM, et al. Comparison of two surgical techniques for the management of cervical spondylomyelopathy in Dobermans. J Small Anim Pract. 1998; 39 (9):425-431.
17. LeMarie, RJ, Kerwin SC, Partington BP et al. Vertebral subluxation following ventral cervical decompression in the dog. Journal of the American Animal Hospital Association 2000; 36,348-358
18. Bruker K, Seim HBI, Withrow S. Clinical evaluation of three surgical methods for treatment of caudal cervical spondylomyelopathy of dogs. Vet Surg 1989a; 18: 197-203.
19. Gilpin GN. Evaluation of three techniques of ventral decompression of the cervical spinal cord in the dog. J Am Vet Med Assoc 1976; 168 (4): 325-328.
20. Trotter EJ. Cervical spine locking plate fixation for treatment of cervical spondylotic myelopathy in large breeds. Vet Surg 2009; 38: 705–718.
21. Dixon BC, Tomlinson JL, Kraus KH. Modified distraction-stabilization technique using an interbody polymethylmethacrylate plug in dogs with caudal cervical spondylomyelopathy. J Am Vet Med Assoc 1996; 208: 61–68.
22. Brucker K, Seim H, Blass C. Caudal cervical spondylomyelopathy: decompression by linear traction and stabilization with Steinmann pins and polymethylmethacrylate. J Am Anim Hosp Assoc 1989b; 25(6) 677-683.
23. Seim HI, Prata R. Ventral decompression for the treatment of cervical disc disease in the dog: a review of 54 cases. J Am Anim Hosp Assoc 1982; 18: 233–240.
24. Ellison GW, Seim HB III, Clemmons RM. Distracted cervical spinal fusion for management of caudal cervical spondylomyelopathy in large-breed dogs. J Am Vet Med Assoc 1988;193: 447–453.
25. McKee W, Lavelle R, Richardson J, et al. Vertebral distraction-fusion for cervical spondylomyelopathy using a screw and double washer technique. J Small Anim Pract 1990;31: 22–27.
26. McKee W, Buttersworth S, Scott H, et al. Management of cervical spondylopathy-associated intervertebral disc protrusion using metal washers in 78 dogs. J Small Anim Pract 1999;40: 465–472.
27. Shamir M, Chai O, Loeb E. A method for intervertebral space distraction before stabilization combined with complete ventral slot for treatment of disc associated wobbler syndrome in dogs. Vet Surg 2008;37: 186–192.
28. Bergman R, Levine J, Coates J, et al. Cervical spine locking plate in combination with cortical ring allograft for a one level fusion in dogs with cervical spondylotic myelopathy. Vet Surg 2008;37: 530–536.
29. Koehler CL, Stover SM, Le Couter RA, et al. Effect of a ventral slot procedure and of a smooth or positive-profile threaded pins with polymethylmethacrylate fixation on intervertebral biomechanics at treated and adjacent canine cervical vertebral motion units. Am J Vet Res 2005;66(4): 678-687
30. Corlazzoli D. Bicortical implant insertion in caudal cervical spondylomyelopathy: a computed tomography simulation in affected Doberman Pinschers. Vet Surg 2008; 37(2): 178-185
31. Hicks DG, Pitts MJ, Bagley RS, et al. In vitro biomechanical evaluations of screw-bar-polymethylmethacrylate and pin-polymethylmethacrylate internal fixation implants used to stabilize the vertebral motion unit of the fourth and fifth cervical vertebrae in vertebral column specimens from dogs. Am J Vet Res 2009;70(6): 719-726
32. Voss K, Steffen F, Montavon PM. Use of the ComPact UniLock System for ventral stabilization procedures of the cervical spine: a retrospective study. Vet Comp Orthop Traumatol 2006;19(1): 21-28
33. Seim HB. Diagnosis and treatment of cervical vertebral instability-malformation syndromes. In. Bonagura JD, ed Kirk’s current veterinary therapy XIII: small animal practice. 13th ed Philadelphia: Saunders, 2009; 992-1000.
34. Van Gundy TE. Disc-associated wobbler syndrome in the Doberman Pincher. Vet Clin North Am Small Anim Pract 1988;18(3): 667-696.
35. Jeffery ND, McKee WM. Surgery for disc associated wobbler syndrome in the dog – an examination of the controversy. J Small Anim Pract 2001;42: 574-581.
36. Wilson ER, Aron DN, Roberto RE, et al. Observation of a secondary compressive lesion after treatment of caudal cervical spondylomyelopathy in a dog. J Am Vet Med Assoc 1994;205: 1297-1299.
37. Adamo PF. Cervical arthroplasty in two dogs with disc-associated cervical spondylomyelopathy. J Am Vet Med Assoc 2011;239 (6): 808-816.
38. Adamo PF, da Costa RC, Giovannella C, et al. 2012. Cervical Disc Arthroplasty in 12 Dogs Affected by Disc Associated Wobbler syndrome: Preliminary Results. In Proceeding. Annu Meet Am Coll Vet Int Med Forum; New Orleans.
39. Adamo PF, Kobasyashi H, Markel M, et al. In vitro biomechanical comparison of cervical disc arthroplasty, ventral slot procedure, and snooth pins with polymethylmethacrylate fixation at treated and adjacent canine cervical motor units. Vet Surg 2007;36: 729-741.
Disc Disease
Disc disease is most prevalent among small and toy breed dogs such as Dachshunds, Lhasa Apsos, Poodles, Beagles and Pekingese dogs. However, there is also a significant occurrence of disc disease in large and giant breed dogs such as Dobermans, Dalmations, Labradors, Mastiffs, St. Bernards, German Shepherds, Rottweilers, and Great Danes as well as cats! In the more prevalent smaller breeds, primarily due to genetic factors, the disc is prone to premature aging thus making them more likely to rupture even with minimal movements. In these genetically predisposed breeds the highest incidence of disc rupture occurs between three and six years of age. Intervertebral discs can rupture either in the middle-back (thoraco-lumbar region) or the neck (cervical spine). Different clinical signs in the effected patient will depend on the site of rupture and the amount of trauma associated with the disc rupture.
The Disc: Anatomy and Pathology
A normal disc resembles a jelly-filled doughnut. The outer layer (the dough) is called the annulus and consists of a tough fibrous tissue that connects each of the spinal vertebrae together into a column. (Fig. 1) Due to the flexibility of the annular fibers, the vertebral column is able to flex and bend. The center of the intervertebral disc (the jelly) is called the nucleus and contains a viscous liquid.
Within degenerating discs (discs susceptible to rupture), the nucleus changes in consistency, becoming denser and more like toothpaste rather than jelly. Simultaneously, cracks will develop in the annulus: when these cracks become sufficiently large or sufficiently weaken the structure, the central nuclear material can herniate (squirt out), resulting in compression and damage to the spinal cord.
Even a small amount of ruptured nuclear material may cause your pet to experience mild to moderate back or neck pain with or without limb weakness (paresis) and unsteadiness (ataxia). Larger quantities of disc material expelled (extruded) at once and with extreme velocity, however, can cause acute loss of control of the legs (paralysis), sudden loss of bowel and bladder function and, in severe cases, difficulty breathing, abnormal heart rhythms and death.
The chance of your pet recovering from a ruptured disc depends on overall medical health, the number of previous episodes of pain or paralysis, and the length of time between the onset of the current problem and the intervention of veterinary care. The best indicator of return to good function is your pet’s neurologic status at the time of surgery.
Myelography
If your pet fails to respond sufficiently to non-surgical, medical management, surgery may be indicated. If so, radiographs (x-rays) and a myelogram are important diagnostic tools to identify the exact location of disc rupture.
A myelogram must be performed with the patient under general anesthesia. A spinal tap is performed and radio-opaque dye is injected around the spinal cord to make its shape visible on radiographs. Following the injection a series of radiographs may indicate which disc has ruptured and delineate the amount of compression of the spinal cord. (Fig. 2) The surgeon can then determine which type of surgical technique to use and where the surgical approach should take place.
Rarely, following a myelogram, a patient may have transient seizures (usually resolving with overnight monitoring and treatment). A more common side-effect of myelography is an increase in limb weakness that may last for as long as one to two weeks. More severe side effects are rare but possible. The benefits of myelography far outweigh these risks and this diagnostic modality still remains one of the most routine tests available to identify a ruptured disc. In some situations, myelograms are slowly being replaced by CT’s and MRI’s. (Figs 3 & 4) However, these alternatives are more expensive, they are not always available on an emergency basis, nights or weekends, and even with these advanced imaging techniques, radio-opaque dye injection may still be indicated.
Disc Surgery: Back
Often, pets with back pain only or minor spinal cord injury can benefit from a fenestration surgery. (Fig. 5) In this procedure, the surgeon cuts a window in the annulus of several discs in the back and removes the inner, abnormal nuclear material that is applying pressure to the spinal cord. This technique removes the nucleus from the currently rupturing disc as well as that of other discs that appear likely to rupture in the future. Unfortunately, this technique is rarely effective in patients with demonstrable disc extrusion.
Instead, paralyzed patients, or patients with demonstrable disc extrusion, are candidates for laminectomy surgery. (Fig. 6) This technique involves removing part of the bony vertebrae surrounding the region of damaged spinal cord. The material extruded from a ruptured disc is removed from around the spinal cord, thus relieving pressure and preventing further trauma. As the swelling in the cord gradually subsides following surgery, some nerve function returns to the legs. It is important to realize that recovery does not happen overnight, and that not all nerve function may recover.
Some pets suffer temporary setbacks in their neurologic status following surgery. These delays relate to the effects of the myelogram, manipulation of the spinal cord during surgery and the progressive swelling and damage from the initial disc rupture. While these setbacks are not usually permanent, they do prolong the patient’s postoperative rehabilitation and require additional efforts by owner, pet and veterinarian alike.
Disc Surgery: Neck
Once a cervical (neck) disc has ruptured, your pet will rarely improve without treatment or surgery. Often, there may be a reduction in the pain by administering anti-inflammatory medications and muscle-relaxants, but steroids are not recommended because of harmful side effects when used long-term. Surgical repair of ruptured cervical discs is generally quite successful.
After the specific ruptured disc is located by myelography or MRI, a ventral cervical slot procedure allows access to the spinal cord and removal of the extruded material. The ventral slot technique relieves pressure from the spinal cord and also fenestrates additional cervical discs to remove abnormal nuclear material and prevent at-risk discs from rupturing in the future. (Fig. 7) The annulus is left intact to stabilize the neck and to allow the vertebrae of the neck to move normally after surgery.
Similar to disc surgery in the back, inflammation and neck pain start to subside once the pressure on the spinal cord is relieved. Some nerve function should start to return and gradual recovery begins.
Postoperative Recovery and Care
After back surgery one should expect approximately four weeks of intensive home nursing care before clinicians may fully determine the outcome of the procedure. During this recovery phase your pet may not have bladder or bowel control and may have no or only partial movement of the limbs. Because of these conditions, the patient will require a great deal of assistance and attention. Our staff will provide you with complete instructions to assist you during this recovery period.
Many paralyzed pets start to move their legs in approximately two to four weeks time. Within four to eight weeks many will regain continence and start to walk. Some pets return to very good hind limb function, while others may have permanent impairments and wobble or have difficulty jumping for the remainder of their lives.
The primary goal of neck surgery is to relieve the pain caused by the ruptured disc and most pets also regain very good motor function. It is important to keep the patient quiet and confined for four weeks following surgery to help with healing and recovery. Again, temporary neurologic deficits may persist and, although generally they are not permanent, they may prolong postoperative rehabilitation.
Ventral Slot Surgery Recovery Centers
In most cases the swelling and pain associated with a ruptured neck disc subside in two to four weeks. If nerve damage also exists, improvement may take four to eight weeks or longer. Decreasing doses of steroids may be administered during this transition to decrease inflammation and associated pain. Even with the most ideal surgical technique and recovery management, it is possible that your pet may not recover full function of the limbs or return to pre-injury functional status.
Remember, regardless of the location along the spine of a disc rupture, the very best indicator of your pet’s chances of recovering full functional status (walking and continence) is the neurologic status at the time of surgery. Fortunately, even pets that remain permanently paralyzed and incontinent, while challenging to care for, can live happy and healthy lives.
Ventral Slot Surgery Recovery Disk
Conclusion
An accurate diagnosis and prognosis for surgical success can be made only after a thorough medical, physical and neurologic examination of your pet. We will discuss our findings and expectations with you to help make the best decisions for your family and for your friend. Please call Veterinary Surgical Centers with any questions or concerns about intervertebral disc disease in your pet.